Improving the ROI of EHRs Through Analytics

Improving the ROI of EHRs Through Analytics
Authored by Ayesha Rajan, Research Analyst at Altheia Predictive Health
Introduction
As with any business feature, business owners and analysts must consider whether or not the cost associated with a feature is worth the return on investment. Electronic Health Records, though an integral part of the healthcare system, are a good example of a staple that does not often justify its cost. EHRs, of course, are extremely beneficial within healthcare, however, their high implementation and maintenance costs (think billions of dollars) means that they are not necessarily worth the investment unless steps are taken to optimize their use. Due to the fact that EHRs are ingrained into our healthcare system, the question isn’t whether or not they are worth the investment but how we can make them worth the investment?
Discussion
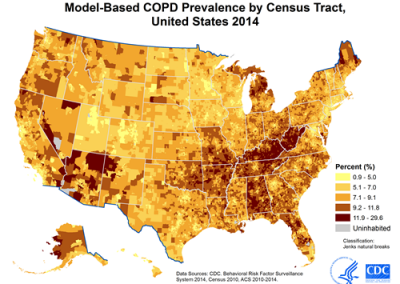
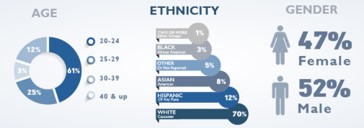
The first and most documented issues with EHRs is their accessibility and readability which limits their usability as well. Additionally, “EHR reports tend to run on a predetermined schedule, limiting how the data within the EHR can be used to evaluate key performance indicators, populations studies, or long-term trends” which further limits their ability to be improved upon. Many investors and market researchers say that the next step in EHR improvement is to invest heavily in programs and softwares that are able to translate the data from EHRs to other softwares so that it can be used across different contexts. This development will allow the power of analytics to significantly improve the return on investment for EHRs by providing insight and direction in terms of bed management, case management, ED, workforce management, scheduling, and OR management systems [such that] staff can see the upstream and downstream effects of a single operational decision.” This is important because the time it takes to “translate” EHR data means that time has passed since data was collected and, in healthcare, real-time insights and decisions can be critical. Once the issue with readability and context application is solved, EHRs can be used to support predictive analytics endeavors by providing on-demand trend analysis and suggested steps to be verified by physicians. Such insight can cut costs for hospitals by tracking patient flow, for providers by creating demographic reports and for patients by reducing the number of tests needed for diagnosis.
Conclusion
The newest development in this space is a Google study’s use of deidentified EHRs to make patient health predictions. Though this project is still in the proof of concept phase, their prediction models have outperformed standard hospital models in every test thus far. This is a promising development in the optimization of EHR use that could encourage further research from smaller companies and at the university level, as well as inspire further investments towards the effort of getting the most out of Electronic Health Records.