August 2025 | Altheia Almanac
Altheia has news to share. Here is our August Newsletter, the Altheia Almanac.
Altheia has news to share. Here is our August Newsletter, the Altheia Almanac.
Altheia is excited to share that the podcast Disruption Interruption recently featured our CEO, Jolly Nanda. Jolly highlights how her own struggles with getting health answers led to the development of our first product, Acuvía.
Acuvía is leveraging the best of AI to break down data barriers and enable health data convergence. Connect with us. Collaborate with us. We’re currently raising funding – invest with us!
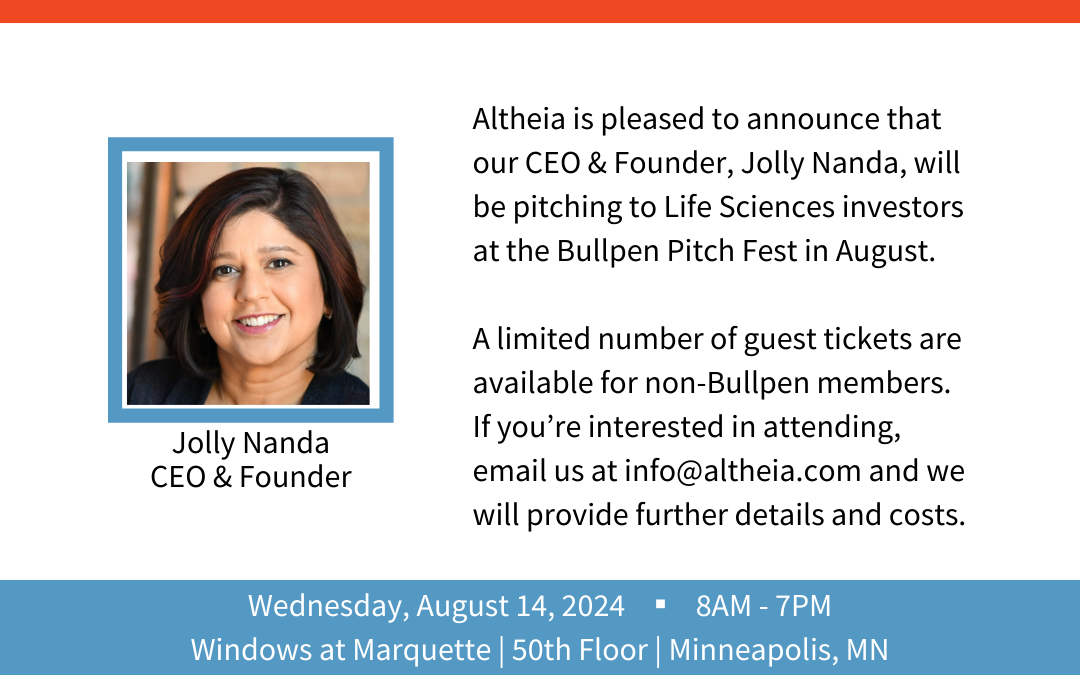
Altheia is pleased to announce that our CEO & Founder, Jolly Nanda, will be pitching to Life Sciences investors at the Bullpen Pitch Fest in August.
A limited number of guest tickets are available for non-Bullpen members for $395 each. If you’re interested in attending, email us at info@altheia.com and we will ensure you receive your guest invitation.

Because we do not have a national healthcare system, we are constantly creating churn given the vast amount of insurance fluctuation. In fact, people change jobs – and therefore health plans – on average 5-7 times in a lifetime. Also, 10,000 people per day age into Medicare. Many have a rotating door going in and out of Medicaid depending on current income levels – resulting in state exchange flux. And every time we change insurance plans or programs, we often change providers given stipulated networks. It would be one thing if everyone was healthy, but these days 60% of the population has at least one chronic condition (40% have two or more) – meaning we are creating care blind spots and care disruptions since there is no seamless integration between systems.
This constant churn translates into unknown risk and potentially unmanaged care for both payers and providers, not to mention the operational inefficiency that comes with these changes:
Again, if everyone in this new member category were healthy, this might not be a big deal – but we all know this is not the case. On average, twenty percent of the population is in the rising or high-risk category – driving 80% of the costs – so care continuation & management is critical since 5-15% of this spend can be managed out. And not only costly, chronic conditions impact absenteeism and productivity even when properly managed – which is all exasperated through non-adherence.
What are new employees/members costing you? How can you target the right folks to fast-track care management and care continuity? What if we armed patients with the data you need to run your business effectively? Let’s not miss an opportunity.